Plasma Therapy Removed From COVID-19 Treatment
Plasma therapy no longer part of Covid treatment, says ICMR
TNI Bureau: In a major decision, India on Monday, removed convalescent Plasma Therapy from the list of country’s treatment protocol for COVID-19 patients in its revised clinical guidelines.
The guidelines jointly issued by the Indian Council of Medical Research (IMCR)-Covid-19 National Task Force, All India Institute of Medical Sciences, Delhi and Union Ministry of Health and Family Welfare.
The decision has been made after an expert group of Indian Council of Medical Research (ICMR) had not found any benefit of the plasma therapy in the treatment process of corona patients.
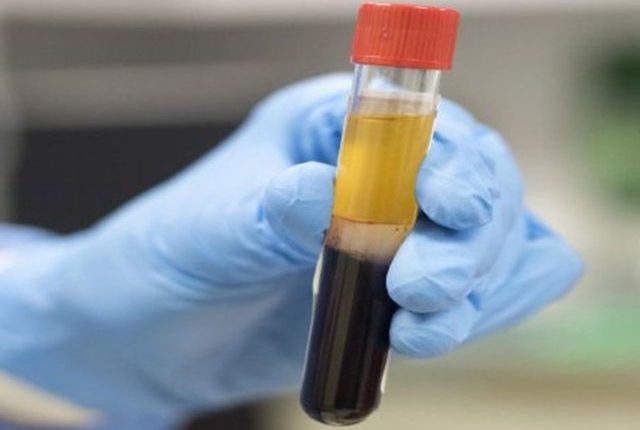
Notably, Plasma therapy is a kind of treatment that uses a blood component called plasma rich virus-fighting antibodies from recovered Covid-19 patients and to develop the immunity system of the body in fighting against the virus. The therapy had been widely used in India to treat COVID-19 patients.
Earlier, India had conducted several studies regarding the efficacy of plasma therapy and in last September the health experts found that plasma therapy failed to save people dying from Covid-19.
Recently, British medical journal, Lancet also published strong evidence re-confirming that plasma is not effective in reducing deaths in Covid-19 cases.
Clinical Guidelines for Management of Adult Covid-19 Patients:
For Mild Disease
The guidelines identify a mild Covid-19 disease with upper respiratory tract symptoms (& or fever) without shortness of breath or hypoxia. Such people should undergo Home Isolation and Care.
Must Dos
• Physical distancing, indoor mask use, strict hand hygiene.
• Symptomatic management (hydration, antipyretics, antitussive, multivitamins).
• Stay in contact with treating physician.
• Monitor temperature and oxygen saturation (by applying a SpO2 probe to fingers).
Seek immediate medical attention if:
• Difficulty in breathing
• High grade fever or severe cough, particularly if lasting for more than 5 days
• A low threshold to be kept for those with any of the high-risk features
For Moderate Disease
A mild disease many have symptoms like respiratory rate more than 24 per minute, breathlessness or SpO2: 90% to less than 93% on room air. Such patients should be admitted in wards.
Oxygen Support:
• Target SpO2: 92-96% (88-92% in patients with COPD).
• Preferred devices for oxygenation: non-rebreathing face mask.
• Awake proning encouraged in all patients requiring supplemental oxygen therapy (sequential position changes every 2 hours).
Anti-inflammatory or immunomodulatory therapy:
• Injection Methylprednisolone 0.5 to 1 mg per kg in 2 divided doses (or an equivalent dose of dexamethasone) usually for a duration of 5 to 10 days.
• Patients may be initiated or switched to oral route if stable and or improving.
Anticoagulation
• Conventional dose prophylactic unfractionated heparin or Low Molecular Weight Heparin (weight based e.g., enoxaparin 0.5mg or kg per day SC). There should be no contraindication or high risk of bleeding.
Monitoring:
• Clinical Monitoring: Work of breathing, Hemodynamic instability, Change in oxygen requirement.
• Serial CXR; HRCT chest to be done only if there is worsening.
• Lab monitoring: CRP and D-dimer 48 to 72 hourly; CBC, KFT, LFT 24 to 48 hourly; IL-6 levels to be done if deteriorating (subject to availability).
Support Independent Journalism? Keep us live.
For Severe Disease
The guidelines identify a severe Covid-19 disease with either Respiratory rate more than 30 per minutes, breathlessness or SpO2 less than 90% on room air.
Respiratory support:
Consider use of NIV (Helmet or face mask interface depending on availability) in patients with increasing oxygen requirement, if work of breathing is low.
Consider use of HFNC in patients with increasing oxygen requirement.
Intubation should be prioritized in patients with high work of breathing or if NIV is not tolerated.
Use conventional ARDSnet protocol for ventilatory management.
Anti-inflammatory or immunomodulatory therapy:
• Inj Methylprednisolone 1 to 2 mg per kg IV in 2 divided doses (or an equivalent dose of dexamethasone) usually for a duration 5 to 10 days.
Anticoagulation
• Weight based intermediate dose prophylactic unfractionated heparin or Low Molecular Weight Heparin (e.g., Enoxaparin 0.5mg per kg per dose SC BD). There should be no contraindication or high risk of bleeding.
Supportive measures
• Maintain euvolemia (if available, use dynamic measures for assessing fluid responsiveness).
• If sepsis or septic shock: manage as per existing protocol and local antibiogram.
Monitoring:
• Serial CXR; HRCT chest to be done only if there is worsening.
• Lab monitoring: CRP and D-dimer 24-48 hourly; CBC, KFT, LFT daily; IL-6 to be done if deteriorating (subject to availability).
As per the guidelines, the high-risk for severe disease or mortality include those who have:
• Age more than 60 years
• Cardiovascular disease, hypertension, and CAD
• DM (Diabetes mellitus) and other immunocompromised states
• Chronic lung or kidney or liver disease
• Cerebrovascular disease
• Obesity
Read More

Comments are closed.